[HGPI Policy Column] (No. 64) From the Dementia Project “Curtailing the Prevalence of Dementia through Evidence-Based Policies addressing Preventable Risk Factors”
date : 10/15/2025
Tags: Dementia, HGPI Policy Column
![[HGPI Policy Column] (No. 64) From the Dementia Project “Curtailing the Prevalence of Dementia through Evidence-Based Policies addressing Preventable Risk Factors”](https://hgpi.org/en/wp-content/uploads/sites/2/Columun-64.png)
<POINTS>
- The identification of modifiable risk factors is key for dementia policies to curtail the increasing prevalence of dementia and a thorough understanding of these risk factors is essential for effective implementation of risk reduction programs.
- Longer exposure to risk factors has a greater effect and increase the onset and prevalence of dementia; therefore, it is essential to comprehend these risk factors and their mechanisms to reduce the duration of exposure.
- There is a need to promote adequate and relevant interventions that are tailored to the needs of the individual and the community, and that are able to weaken the impact of the risk factors resulting in dementia.
- The challenges facing prevention and risk reduction such as life-long exposure to risk, the effect of long prodrome before identification, diversity, equity and inclusivity as well as the disparity between HIC and LMIC.
- Real-world evidence driven policies that put emphasis on modifiable and preventable risk factors through a life-course approach, a public health approach, and timely diagnosis are warranted.
Introduction
The Lancet Commission recently published their 2024 report of dementia prevention, intervention and care titled ‘Dementia prevention, intervention, and care: 2024 report of the Lancet standing Commission’. This report is an updated version of the 2020 report which we summarized in the column titled ‘Considering the risk factors for dementia, the importance of addressing dementia issues through multi-stakeholder and global efforts.’ Alongside the thorough evaluation of additional studies since 2020, the 2024 Commission report accentuates notable new topics, such as the need for a personal and a population-level response to dementia risk reduction that addresses health equity, discussion of emerging treatments, and developments in care. As a result, this report is expected to and is likely to raise awareness of the importance of risk reduction as well as underline the impact of policy intervention and personalized risk reduction programs globally.
Methodology
In comparison to the 2020 report, the 2024 is underpinned by a more thorough and comprehensive analysis of the 14 modifiable risk factors for dementia as it updates previous calculations with new risk factors and worldwide estimates of relative risk (RR) and prevalence for the risk factors. Additionally, systematic reviews were used for the chosen risk factors, and new meta-analysis were conducted where required for data synthesis. In order to calculate the total population attributable fraction (PAF) for the prevalence of the risk factors that lead to dementia, 2 new risk factors (untreated visual loss and high LDL cholesterol) were added to the 12 risk factors (social isolation, air pollution, depression, obesity, traumatic brain injury, physical inactivity, diabetes, smoking, hypertension, excessive alcohol consumption, low education level) already stated in the 2020 report. To evaluate the 14 risk factors, data from 37,000 participants aged 45 and older from a longitudinal, population-based study from Norway was employed.
It is necessary to note that the identification of these risk factors is key for dementia policies to curtail the increasing prevalence of dementia. A thorough understanding of these risk factors is essential for effective implementation of risk reduction programs.
Risk Factors for Dementia Prevention
For dementia policies, intervention and care to be impactful, evidence-based, citizen-centered policies are warranted. Policies affect people’s lives, health policies influence the lives of people living with illness and could impact the provision and access to adequate diagnosis, treatment, and prevention. Thus, the voices of people living with illness in healthcare policy formation is indispensable. This point is also emphasized in the 2024 Lancet Commission report. The 2024 report is an update of the 2020 report, however, with some novelties. This report emphasizes that longer exposure to risk factors has a greater effect and increase the onset and prevalence of dementia. Moreover, risk factors act differently in different individuals such that they exert a stronger effect in vulnerable individuals from socially disadvantaged background. As well as this, regarding preventative risk factors, two new risk factors, namely high LDL cholesterol and untreated vision loss were added to the list after thorough consideration and analysis. Both high and low cholesterol are modifiable risk factors for dementia. Recent research has revealed that excess brain cholesterol is associated with increased stroke risk and deposition of brain amyloid β and tau, suggesting a potential mechanism for the link between LDL cholesterol and dementia.
Furthermore, the relationship between untreated visual loss and dementia prevalence is still being investigated. However, the underlying mechanisms behind this association may be related to underlying illness, or shared neuropathological processes in both the retina and the brain.
This report also underlines the promotion of adequate and relevant interventions that are tailored to the needs of the individual and the community. Multinational, multidisciplinary and multi-sectoral initiative are required to provide novel and appropriate solutions for the diagnosis, treatment and prevention of dementia. New directions for the field include precision prevention therapies such as the use of blood-based biomarkers for early detection of individuals at risk; combination therapies involving both tailored multidomain lifestyle-based interventions, which should consider urban environments that might facilitate or hinder the adoption of healthy lifestyles, and pharmaceutical treatments.
In addition to these newly added risk factors, the challenges facing prevention and risk reduction such as life-long exposure to risk, the effect of long prodrome before identification and diversity, equity and inclusivity were also underlined in this report. Another challenge is the disparity between high-income countries (HIC) and low-middle income countries (LMIC). Due to this disparity, treatment, prevention and intervention have must be tailored to the context. Moreover, the majority of the studies and outcomes that have been reported are from HIC; applying these outcomes in LMIC without understanding the cultural and sociopolitical context would be inefficient. Therefore, it is crucial to understand the cultural and sociopolitical context in LMIC and promote research from this context to promote diversity, equity and inclusivity in the field of dementia research.
Figure 1: Summary of the potential mechanisms of protection from dementia
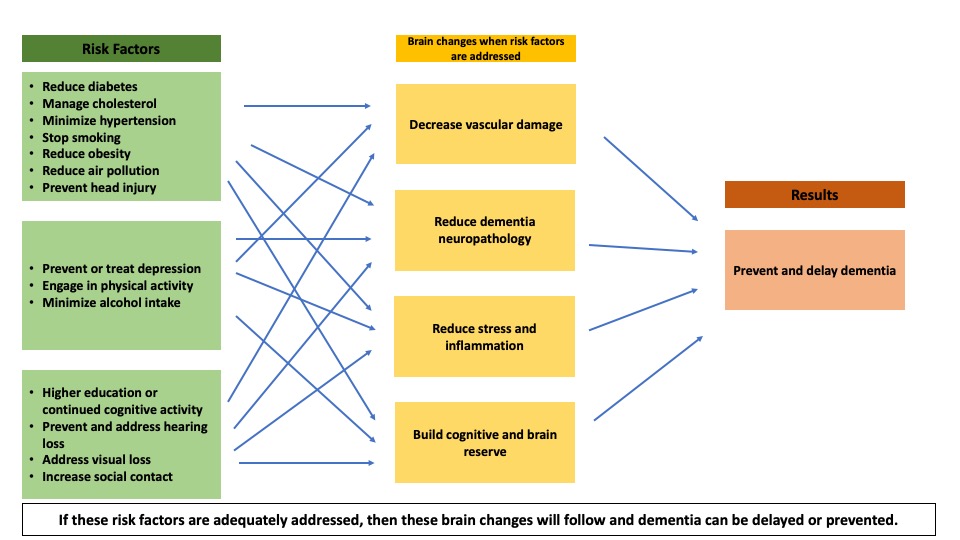
Figure 1 displays the summary of the potential mechanisms for maintaining and enhancing cognitive reserve and reinforcing risk reduction of the modifiable risk factors in dementia.
Figure2: Population attributable fraction of potentially modifiable risk factors for dementia
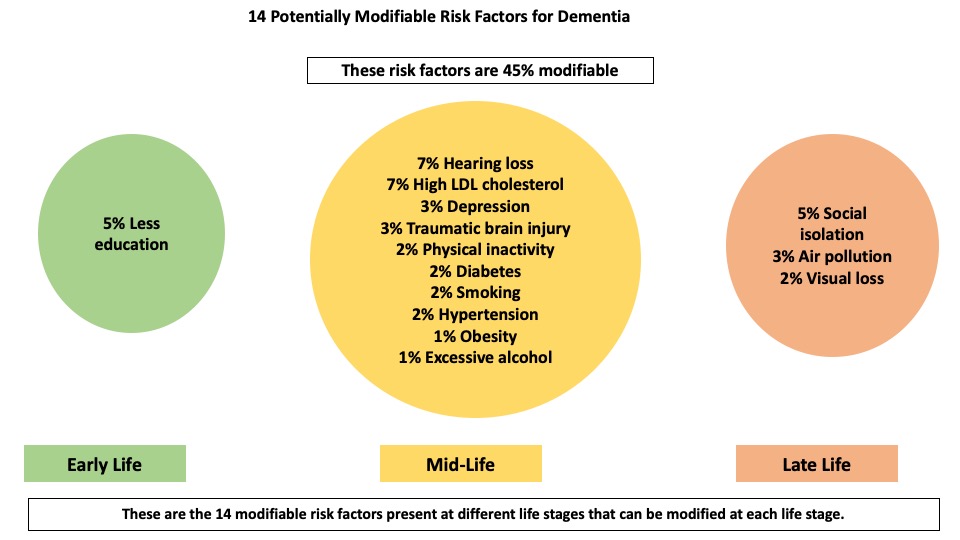
Figure 2 shows the life-course model of 14 potentially modifiable risk factors for dementia.
Call to Action
The call to action from this report is the emphasis on modifiable and preventable risk factors through a life-course approach, a public health approach, and timely diagnosis. This report encourages dementia prevention and risk reduction through a life-course approach by underlying that some risk factors can be prevented at different stages of life. For example, a low level of education can be prevented early in life, lifestyle risk factors such as physical inactivity and excessive alcohol consumption can be prevented in midlife, factors like social isolation and visual loss can be prevented in the later stages of life.
Additionally, a public health approach to preventing dementia is also presented in this paper. Although dementia is a leading public health challenge, a public health approach to curtailing the prevalence of dementia is quite a novel approach. Risks can be conceptualized and understood as factors for which every individual can change; however, a public health approach recognizes the influence of the social economic background of an individual on their health, and the life-course generation of ill health. The public health approach facilitates the comprehension of health inequity and the causes of risk inequalities, such as unequal access to healthy environments, deprived occupational conditions and unequal access to education. The understanding of these causes alongside real-world data centered on the voices of the individuals most afflicted by health inequalities can compel the formation of policies that will result in reforming societal conditions to maximize population reach, cost-effectiveness, and health equity of interventions.
To adequately prevent dementia, timely diagnosis is warranted. Timely diagnosis if dementia has to be a priority because diagnosis will determine treatment, prevention and prognosis. To establish early and appropriate diagnosis, barriers that hinder diagnosis such as denial, stigma, lack of knowledge and unawareness of symptom development etc., need to be addressed through a multisectoral, multidisciplinary and multinational approach centered on the voices and experience of individuals living with dementia.
Conclusion
In conclusion, the number of people with dementia will continue to rise globally; therefore, global and local action through evidence-based, citizen-centered policies, need to be promoted and taken to tackle the increasing prevalence of dementia. This report highlights what the central focus of policy makers, healthcare professionals, researchers and patients living with dementia should be; taking measures to reduce the prevalence of modifiable risk factors. It is crucial that policy makers prioritize resources to enable risk reduction to prevent or delay dementia and promote interventions to improve symptoms and life for people living with dementia, their families and caregivers. The prevention approach should be grounded in real-world data from those living with dementia and directed at addressing risk factor levels at an early stage and continuing throughout the life course.
Based on Japan’s Basic Act on Dementia, HGPI will continue to promote integrated, action-oriented outcomes centered on equity. These outcomes will ensure that dementia risk reduction measures respect individual autonomy and promote evidence-based, citizen-centered policies.
Column author
Favour Omileke (Program Specialist, Health and Global Policy Institute)
Top Research & Recommendations Posts
- [Research Report] Perceptions, Knowledge, Actions and Perspectives of Healthcare Organizations in Japan in Relation to Climate Change and Health: A Cross-Sectional Study (November 13, 2025)
- [Research Report] The 2025 Public Opinion Survey on Healthcare in Japan (March 17, 2025)
- [Policy Recommendations] Developing a National Health and Climate Strategy for Japan (June 26, 2024)
- [Research Report] The 2023 Public Opinion Survey on Satisfaction in Healthcare in Japan and Healthcare Applications of Generative AI (January 11, 2024)
- [Research Report] Survey of Japanese Nursing Professionals Regarding Climate Change and Health (Final Version) (November 14, 2024)
- [Policy Recommendations] Mental Health Project: Recommendations on Three Issues in the Area of Mental Health (July 4, 2025)
- [Policy Recommendations] Reshaping Japan’s Immunization Policy for Life Course Coverage and Vaccine Equity: Challenges and Prospects for an Era of Prevention and Health Promotion (April 25, 2025)
- [Publication Report] Planetary Health Promotion Project “Issues Facing Planetary Health and the Role of the Health Sector” (May 10, 2023)
- [Research Report] Survey of Japanese Physicians Regarding Climate Change and Health (December 3, 2023)
- [Announcement] HGPI Joins Global Green and Healthy Hospitals (August 1, 2023)
Featured Posts
-
2025-11-13
[Registration Open] (Webinar) The 1st J-PEP Seminar – Initiating Policy Advocacy from Meaningful Involvement (December 8, 2025)
![[Registration Open] (Webinar) The 1st J-PEP Seminar – Initiating Policy Advocacy from Meaningful Involvement (December 8, 2025)](https://hgpi.org/en/wp-content/uploads/sites/2/mip-ncd-20251208-top.png)
-
2025-12-01
[Policy Recommendations] Recommendations on Strategic Investments in Policies for Brain Health to Revitalize Japan: Hopes for the New Administration (December 1, 2025)
![[Policy Recommendations] Recommendations on Strategic Investments in Policies for Brain Health to Revitalize Japan: Hopes for the New Administration (December 1, 2025)](https://hgpi.org/en/wp-content/uploads/sites/2/HGPI_20251201_Recommendations-on-Strategic-Investments-in-Policies-for-Brain-Health.png)






